a blood test for breast cancer
by Anna Simon
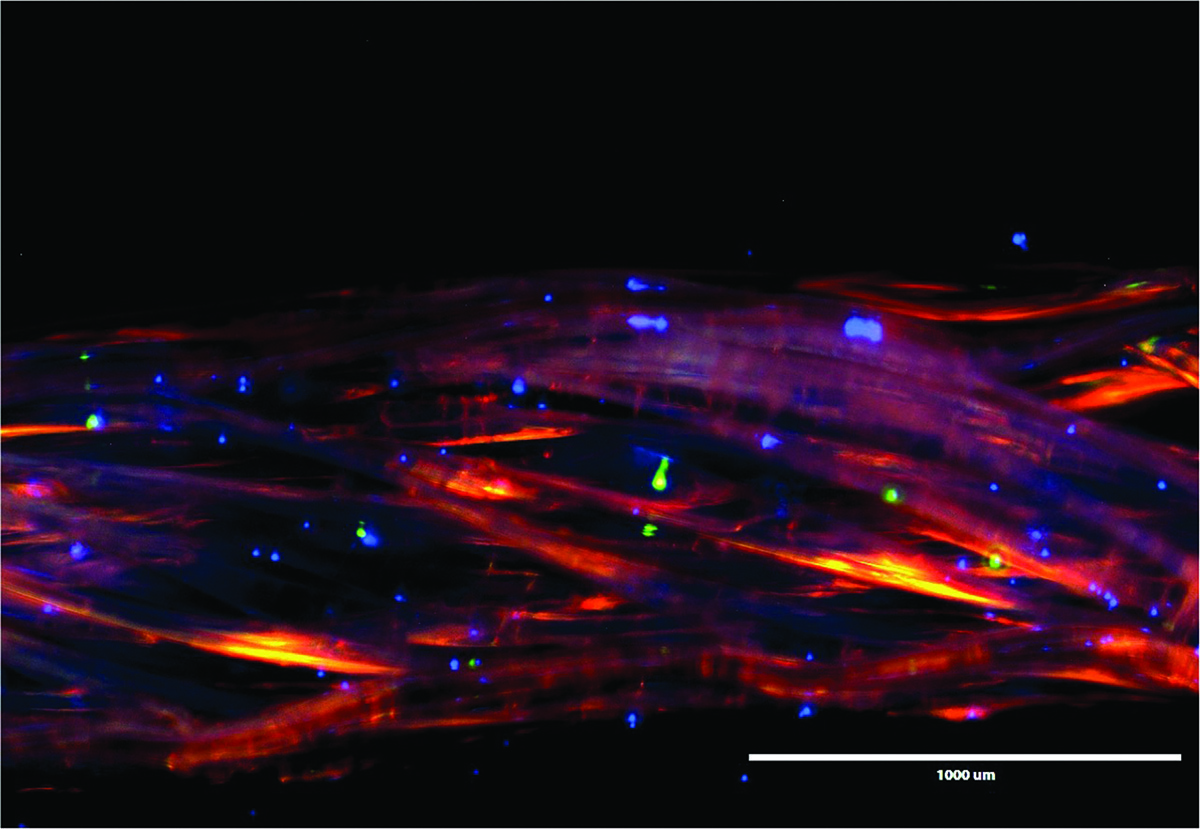 Fluorescent image of cancer cells on specially shaped fibers. The glowing red dots are human breast cancer cells, the blue dots are human breast metastatic cancer cells, and the green are human benign breast epithelial cells. Image by Suzanne Tabbaa.
Fluorescent image of cancer cells on specially shaped fibers. The glowing red dots are human breast cancer cells, the blue dots are human breast metastatic cancer cells, and the green are human benign breast epithelial cells. Image by Suzanne Tabbaa.My mother, Faye Simon, was a breast cancer survivor. The cancer returned years later and took her life. My dad uttered only five words as we left the funeral home: “Cancer is a cruel disease.”
Suzanne Tabbaa envisions the day when a routine blood test would catch breast cancer before it spreads and could help doctors monitor cancer cells during treatment.
As Tabbaa works in labs on the fourth floor of the Rhodes Research Center to develop this diagnostic tool, she describes a family friend who lost her life to cancer. Her friend’s mom had shown no symptoms when a routine exam led to the discovery of Stage IV cancer. It already had “spread everywhere,” Tabbaa says.
Could Tabbaa’s research have helped her friend or my mom? I don’t know. Success so far in research holds hope for early detection and noninvasive monitoring of treatment for future breast cancer patients.
Each year more than 200,000 cases of breast cancer are diagnosed in the U.S. and more than 40,000 people die of the disease, according to the Centers for Disease Control and Prevention. While breast cancer is the most common cancer in women, the statistics also include men.
The blood test would be a simple screening, like the blood tests that millions of Americans undergo regularly to check on cholesterol, iron, and other health markers, Tabbaa says. The test could be done from the same blood sample as those routine screenings.
It would be a simple tool for early detection, to catch recurrences, provide a noninvasive alternative to tissue biopsies, and help doctors see if treatment is working, Tabbaa says.

Suzanne Tabbaa was trying to boost the blood supply to bone grafts when she noticed that the fibers she was using wicked cancer cells. Photo by James Turner.
Medical research with textile roots
Tabbaa started this research as a doctoral candidate and graduate research assistant in Clemson’s Institute for Biological Interfaces of Engineering. She graduated in December 2014 and continues her work as a postdoctoral bioengineering researcher at the institute. The process is rooted in Clemson textile research. “We’re basically taking a method from the textile industry and using it as a cancer diagnostic,” Tabbaa says.
Wicking fibers are used to transport fluid and capture cancer cells that are in the fluid, Tabbaa explains. These fibers are grooved and rough to the touch. The shape is part of the formula that makes the process work, a design donated to Clemson by Eastman Chemical Company. Tabbaa stops at an extruder, a piece of machinery that makes the specially shaped fibers. She hands me a piece of material that looks and feels like a strand of uncooked spaghetti with irregular notches hacked into it.
Several strips of this material extend from a well of liquid on the counter of another lab. Cells that have been placed in this liquid nutrient solution are able to travel up the fibers, Tabbaa says. She uses the fibers to separate cancer cells from normal cells, capturing the cells in a special cap that is the heart of a Clemson patent application for the process.
Physical differences between normal cells and cancer cells keep benign cells from traveling as far as the cancer cells, which are smaller and “squishier,” enabling them to move farther along the wicking material, Tabbaa explains. The process also separates nonmetastatic cancer cells—those that might be in a tumor but either haven’t migrated yet or don’t have the capacity to migrate—from metastatic cells. The metastatic cells travel the longest distance on the highway of absorbent fiber placed in the beaker, Tabbaa says. Each of the three types of cells—benign, nonmetastatic, and metastatic—can be identified by protein markers expressed along the wicking fiber.
We walk down the hall to another lab. Tabbaa places a sample under a microscope and turns off the overhead lights. Normal cells glow green, nonmetastatic cancer cells glow red, and metastatic cells glow blue on a computer screen that shows what Tabbaa sees through the microscope.
Bone-graft work yields a surprise
Tabbaa stumbled upon the possibility for a blood test for breast cancer through earlier work on bone-graft material. She was looking for a way to get blood flow, which carries necessary nutrients, to the central core of large bone grafts such as spinal fusions and large fractures. She investigated the use of wicking fibers as a synthetic vascular system to carry blood to the center of the grafts.
“I started looking at bone cells moving through a wicking process and that led us to wonder how cancer cells move,” Tabbaa says.
Tabbaa discussed applying the wicking fiber technology as a blood test for breast cancer with her mentor, breast cancer tissue researcher Karen Burg. It seemed to make sense, and Tabbaa’s research took a turn.
The patent application filed by Clemson includes processes applicable to diagnostic blood tests and tissue engineered bone grafts, Tabbaa says.
So, when could this blood test be available at your local doctor’s office? It’s generally difficult for researchers to predict when a technology could move from the lab to the marketplace. There are a lot of ifs. Maybe five years, maybe ten, if all goes well, Tabbaa says.
When that time comes, Tabbaa has a marketing plan. She has developed a four-year process to put low-cost test kits, priced at about $10, on the market for clinics and other medical care providers. In April of 2014, her plan won the first place audience award and second place judges’ award at a Society for Biomaterials annual conference business plan competition. The day when she can put that plan into action is still a ways down the road.
The next steps are to move from liquid solution to blood, and then to actual patient blood samples. Clemson received a $150,000 grant from the Avon Walk for Breast Cancer to further this research. The grant abstract states that this “clinically applicable, easy-to-use diagnostic test” is “predictive of breast cancer risk and can be used to monitor breast cancer changes over time.”
When Tabbaa went to an Avon Walk for Breast Cancer event in Charlotte to receive the grant, she was further motivated by the personal stories she heard from the breast cancer survivors and patients she met there. “It’s seeing the application and knowing that you have a chance to help people through your work,” Tabbaa says.
Suzanne Tabbaa was awarded a Ph.D. in bioengineering in December 2014. Her advisor, Karen Burg, is now vice president for research at Kansas State University. At Clemson, Burg was the Hunter Endowed Chair, a professor of bioengineering, and a professor of electrical and computer engineering, in the College of Engineering and Science.
Information about technology from Tabbaa’s work is available from the Clemson University Research Foundation (CURF). CURF is a 501(c)(3) nonprofit corporation dedicated to maximizing the societal impact of Clemson University research through commercialization of intellectual property. For more information on CURF and a portfolio of technologies available for licensing go to clemson.edu/curf.