Repairing a stroke-damaged brain

Natasha Topoluk in the lab: cautious optimism from early results. Photo by Neil Caudle.
So far, stroke is catastrophic. It torches a part of the brain, kills the tissue, and leaves nothing but a gap, an empty hole. The hole does not heal; the tissue does not regenerate. If we’re lucky, brain cells may wire around the hole—neurons connecting new pathways. Sometimes, patients can regain some function. Too often, they can’t.
As of today, there is only one FDA-approved clinical treatment, an enzyme known as tissue plasminogen activator (TPA). It’s useful for only one type of stroke, and very few patients qualify. For the vast majority of stroke victims, a hole in the brain is for keeps. And so far, all attempts to fill that hole have failed.
Natasha Topoluk would like to change that, and she’s off to a good start. Topoluk, a Ph.D. student working with Dan Simionescu, got her first taste of research as an undergraduate working with Agneta Simionescu, helping James Chow with diabetes studies in Aggie’s lab (see defending implants from diabetes). Later, Topoluk set up shop next door, in Dan’s lab, for her graduate work.
Now, with a brand-new master’s degree in bioengineering from Clemson, and a Ph.D. in the game plan for 2016, Topoluk and her mentors may succeed where a great many others have failed. Last summer, she and the neurosurgeon who advises her, Dr. Alfred Nelson (see surgeons help guide the research), implanted what Topoluk calls constructs—matrix scaffolds seeded with stem cells—into the brains of three rats with strokes so severe they could not walk.
When I ask her what happened, she takes her time to get the wording right. Speaking with the confidence of a seasoned pro, she says, “We saw almost complete recovery in our animals less than four weeks after implantation.”
All three rats, rendered helpless by stroke, started to walk little by little. In less than a month, they regained some of their motor functions and some reflexes. The rats in the control group—which did not receive the construct—did not. So far as we know, no one else has done this experiment. Research groups elsewhere have been injecting stem cells into stroke-damaged brains, but most of the cells do not engraft and eventually die, never yielding neural tissue. Other researchers are using gels to try and hold the cells in place. But gels are not the stem cells’ native habitat; the matrix is. So Topoluk and Dan Simionescu are convinced that a matrix seeded with stem cells is a better way to regenerate tissue, even in the brain.
“With the matrix, you can probably keep a cell population in place,” Topoluk says. “Then it just becomes a question of how to manipulate that cell population to take on neural-cell characteristics. I’m making it sound simple, and it’s not simple, but that’s the idea.”
The results so far represent an auspicious beginning, but they are not sufficient, if the goal is to help human patients. The research team, Dan Simionescu says, “is cautiously optimistic,” but no one is drawing any firm conclusions before the next rounds of animal studies. Topoluk wants to know exactly what happened in the brains of those rats. Did the stem cells in fact transform themselves into neurons, or recruit new cells into the matrix? Did the regenerated neurons connect with the brain cells around them, restoring the pathways demolished by stroke?
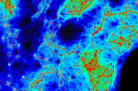
To answer those questions, Topoluk is analyzing the brain tissues, studying the implant areas for proteins expressed by neural cells, which would indicate that stem cells had indeed served a regenerative function in the rats’ brains. In the next phase, she will run more experiments, with greater numbers of rats, for statistical significance and to see if she gets the same results. Nelson has agreed to continue to help her.
“We really lucked out with Doctor Nelson,” Topoluk says. “He did the implants, he’s on my thesis committee, and he even takes the time to review our grant applications. He is so enthusiastic and just genuinely interested in what we do.”
This spring, Topoluk began an internship with Nelson’s department in the Greenville Health System, learning how neuroscience works from the clinician’s point of view. Other Clemson students with similar internships have actually scrubbed in to observe surgery in the operating room, and Topoluk hopes to do that too.
“If we can see firsthand what the clinical setting is actually like, then we can better target our protocols and our approaches to get there one day,” she says, “so that what we make is actually useful to doctors and surgeons.”
Research with laboratory animals, for Topoluk’s studies as well as others in the Simionescus’ labs, was conducted in collaboration with the Godley-Snell Research Center, headed by John Parrish, university veterinarian. The center includes two surgery rooms and complete facilities for housing and treating laboratory animals.